What are cancer biomarkers?
Biomarkers are naturally occurring molecules that can be used as indicators of a normal biological process or a disease state. This makes them valuable tools for diagnosis and prognosis, as well as for establishing whether a chosen course of treatment is effective. By comparing biomarker expression between different sample types, researchers can unravel the complex mechanisms underlying disease development and progression.
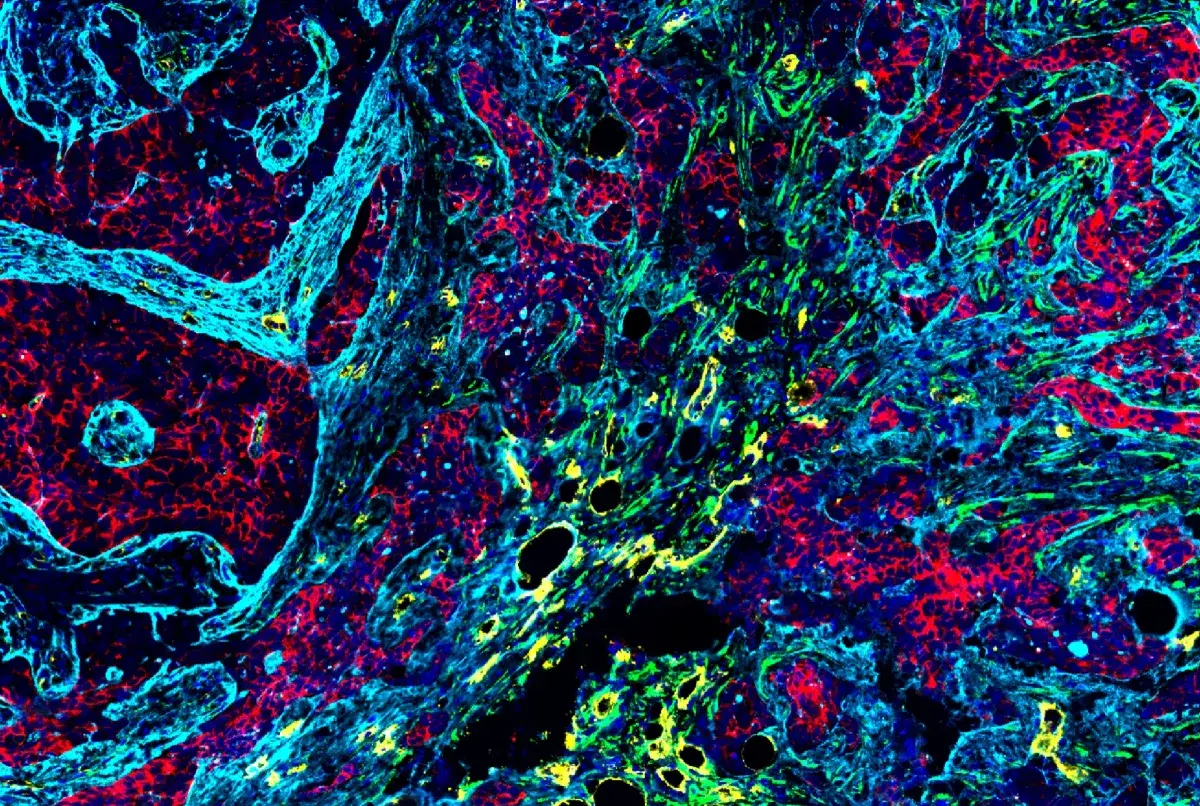
Within the field of cancer research, biomarkers are detected using a broad range of immunoassay techniques. Among these, immunohistochemistry (IHC) is especially advantageous since, unlike methods that require samples to be lysed for analysis, it provides spatial context to a tumor and the surrounding tumor microenvironment (TME). For this reason, IHC promises to reveal novel insights based on biomarker expression and localization.
Accurately detecting biomarkers by IHC requires highly specific, rigorously validated antibody reagents. To safeguard the quality of all our antibodies, CST adheres to the Hallmarks of Antibody Validation, a set of complementary strategies for confirming the specificity, sensitivity, and functionality of an antibody in any given assay. By carefully tailoring how we validate our cancer biomarker antibodies for IHC, we ensure results you can trust.
Types of Cancer Biomarkers
Often, cancer biomarkers provide a direct readout of a specific cancer type or are involved in driving cancer development. Well-known examples are human epidermal growth factor 2 (HER2/ErbB2), which has become an important therapeutic target for many breast carcinomas, and programmed death ligand 1 (PD-L1) which is routinely used to determine whether a patient will benefit from treatment with an immune checkpoint inhibitor.
 IHC analysis of paraffin-embedded human prostate carcinoma using recombinant monoclonal antibody HER2/ErbB2 (D8F12) XP® Rabbit mAb #4290 performed on the Leica BOND Rx. IHC analysis of paraffin-embedded human prostate carcinoma using recombinant monoclonal antibody HER2/ErbB2 (D8F12) XP® Rabbit mAb #4290 performed on the Leica BOND Rx. |
 IHC analysis of paraffin-embedded human non-small cell lung carcinoma using recombinant monoclonal antibody PD-L1 (E1L3N®) XP® Rabbit #13684 mAb performed on the Leica BOND Rx. IHC analysis of paraffin-embedded human non-small cell lung carcinoma using recombinant monoclonal antibody PD-L1 (E1L3N®) XP® Rabbit #13684 mAb performed on the Leica BOND Rx. |
Other cancer biomarkers detected by IHC include markers of lymphocyte or myeloid cell phenotype and function that can be used to localize different immune cells within a tumor and the surrounding tumor microenvironment. These are commonly studied alongside TME markers like fibronectin or keratin to better understand how cancer impacts blood vessels, fibroblasts, or extracellular matrix (ECM) material.
Detecting markers of epithelial to mesenchymal transition (EMT) by IHC is essential to assess cancer progression. During EMT, an epithelial cell loses its polarity and the capacity for cell-cell adhesion and subsequently develops a mesenchymal phenotype characterized by migratory and invasive properties. This enables metastasis, making it vital to monitor the extent to which EMT is taking place. Tumor aggressiveness can also be evaluated by detecting markers of proliferation, cell death, or cell cycle arrest, since dysregulated cell proliferation and apoptosis are classic hallmarks of cancer.
Uncontrolled cell growth is another well-documented cancer hallmark. It is frequently associated with the mutation or deletion of tumor suppressor genes that function to slow down cell division, repair DNA damage, and promote apoptosis. Using IHC to monitor tumor suppressors allows researchers to investigate the role of these proteins in cancer development and metastasis, and in promoting resistance to therapeutic intervention.
Antibody Selection for Cancer Biomarker Research
The Cancer Biomarkers Guide for IHC eBook groups the most critical biomarkers for cancer research into seven categories to streamline antibody selection and emphasize the importance of studying multiple biomarker types in parallel.
Whether you’re investigating the role of immune cells in cancer development and progression, studying lung or breast cancer, or researching classic cancer hallmarks such as uncontrolled cell growth, you can find the right antibodies for your research by biomarker or tissue/organ type in the Cancer Biomarker Guide for IHC eBook: