Dementia is an inevitable burden for many, prevailing under a broad umbrella not only in neurological disorders but also as the natural process of aging. Alzheimer’s disease (AD) represents the most common disease with several stages of dementia, which progresses over time. There are no tools or therapies to cure, prevent, or slow the progression of AD.
Few diseases could generate more apprehension and sadness than AD. Well over 40 million people worldwide are estimated to have symptomatic AD, and perhaps two or three times that number may currently be in the pre-symptomatic/asymptomatic phase, many suffering cognitive deficits with a rapid decline leading to the inability to talk, walk, eat, and soon after, die of systemic complications. A projected 130 million people will be affected by AD by the year 2050 (Figure 1).
 Figure 1. Projected number of people affected with Alzheimer’s disease in the US by the year 2050. Colors represent the range of years old population with Alzheimer’s dementia.
Figure 1. Projected number of people affected with Alzheimer’s disease in the US by the year 2050. Colors represent the range of years old population with Alzheimer’s dementia.
Moreover, in the US, the economic burden of Medicare and Medicaid alone is projected to be 7.58 trillion dollars by 2050. This disease affects not only patients, but also families and care providers, increasing the health and economic burden if a cure or preventive therapies do not improve in the near future. According to economic analysis in the World Alzheimer Report 2015, AD disproportionately affects those of lower socioeconomic status, which do not have the means to manage this disease (Figure 2). The analysis suggests that two-thirds of the population in low and middle income countries will be affected with AD by 2050.

Figure 2. Projected number of Alzheimer’s disease cases by socioeconomic populations by the year 2050. World Alzheimer Report 2015. Alzheimer’s Disease International.
Developing Treatments for Alzheimer’s Disease
While there have been significant advances in the development of treatments some neurological diseases, therapies for AD are lacking. The ideal approach to treat AD would include the detection of appropriate biomarkers at pre-symptomatic stages of the disease (Figure 3), and the development of therapies to stop, or significantly slow, the progression of the disease before the cognitive impairment. Thus, the identification of reliable biomarkers represents the ultimate “holy grail” of Alzheimer’s research, which so far remains elusive despite the advances in the field of neurodegeneration.
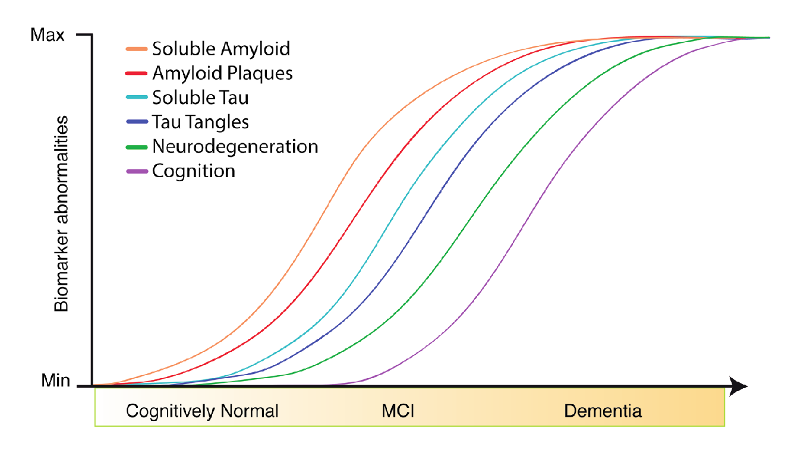
Figure 3. Adapted from Jack CR et al. Lancet Neurology 2013
Current Therapeutic Approaches: Amyloid Plaques & Neurofibrillary Tangles
Historically, research into the biological mechanisms of Alzheimer's disease has focused on the age-related aggregation of toxic proteins, including amyloid plaques made of amyloid β-protein (Aβ) and neurofibrillary tangles (NTF) made of the tau protein. These deposits mainly affect neurons in the central nervous system; however, the presence of Aβ and tau also affects other brain cells, including microglia and astrocytes.
Blog: Unraveling Alzheimer’s Disease: Developing a P-Tau 217 Antibody
There are six isoforms of tau expressed in neurons, including three isoforms with three microtubule-binding domains (isoforms 2, 4, and 5) known as Tau 3R; and three isoforms with four microtubule-binding domains (isoforms 6, 7, and 8) known as Tau 4R. These domains allow tau to stabilize the cytoskeleton of neurons and facilitate the formation of synapses. In addition to these functional properties, tau undergoes many post-translation modifications, mainly phosphorylation, at a wide range of amino acid residues in both normal and AD brains. Several sites are phosphorylated only in the AD brain, including amino acid residues in the microtubule-binding domains. The latter opens up significant opportunities to pinpoint biomarkers in the early stages of the disease, with the potential therapeutic approach to AD.
The effort to find and validate disease-modifying therapies has not yet led to approvable agents, and there is an urgency, and understandable controversy, about how best to achieve this ideal milestone. Thus, the greatest task for scientists is to develop non-invasive and inexpensive systems and approaches to detect biomarkers for AD and focus on tracking patients from the very early stages of the disease, ideally in pre-symptomatic/asymptomatic individuals with a family history of the disease. Having this information will lead to a better therapeutic approach for patients suffering from this disease.
Several pre-clinical and clinical studies have successfully targeted Aβ by using monoclonal antibodies that trap this protein before it spreads to neighboring neurons, thus stopping the propagation of the pathology. The endpoint of this approach is to measure changes in brain activity by positron emission tomography (PET). In a very recent finding, the US Food and Drug Administration approved Ely Lilly’s Tauvid (flortaucipir F18); a drug that detects aggregated tau in NFT and can be measured by PET in live brains from AD patients. This is a major step towards understanding tau pathology in patients; however, this is a very expensive imaging technique to measure pathological tau in pre-symptomatic and clinically diagnosed AD patients. It is not currently the main protocol to detect changes associated with AD.
On the other hand, it has been proven in many studies that levels of tau and Aβ can be detected in the cerebrospinal fluid, or CSF, from individuals with AD, which increases as the disease progresses, suggesting these proteins can be considered biomarkers for AD. However, CSF collection is an invasive and expensive procedure that cannot be performed regularly in AD patients.
While these techniques represent a valuable approach to detect AD features in patients, it is generally understood that a non-invasive blood biomarker for screening in preclinical stages would be crucial for future therapy, as they are easy to perform in longitudinal studies. This is especially true in the context of AD clinical trials, where the move towards early intervention also presents a problem—reliably identifying participants with a high risk of neurodegeneration and cognitive decline throughout a relatively short clinical trial.
Additional Resources:
- Read part 2 of this blog series to learn more about efforts to develop biomarkers for AD.
Select References:
- Mattsson N, et al. CSF biomarkers and incipient Alzheimer’s disease in patients with Mild Cognitive Impairment. CSF Biomarkers and Alzheimer’s disease. 2009.
- Tauvid approved by FDA imaging tau pathology by PET.
- Leuzy A, Heurling K, Ashton NJ, Schöll M, Zimmer ER. In vivo Detection of Alzheimer's Disease. Yale J Biol Med. 2018;91(3):291-300. doi:10.1371/journal.pone.0038284.
- Barthélemy NR, et al. Cerebrospinal fluid phospho-tau T217outperforms T181 as a biomarker for the differential diagnosis of Alzheimer’s disease and PET amyloid-positive patient. Alzheimer’s research and Therapy. 2020.







